Choosing the right behavioral health RCM software can feel complex. The stakes are high, since your revenue cycle touches patient intake, eligibility verification, claims processing, payment posting, and reporting. This guide gives you a clear decision framework, so you can compare platforms, reduce claim denials, and protect cash flow without guesswork.
What makes behavioral health RCM unique?
Behavioral health has workflows and payer rules that differ from general medical billing.
- Care models and treatment plans: Services often include recurring individual therapy, group sessions, IOP, MAT, and community-based care. Treatment plans evolve, and relevant diagnoses can change over time. RCM must link clinical data to the right CPT, modifiers, and payer specific rules.
- Documentation and consent: Accurate documentation, consent management, and managed care authorizations are common. Systems should minimize errors while keeping data security aligned to the HIPAA Security Rule.
- Complex billing codes and coverage: Benefits differ for mental health services, mental illness screenings, medication assisted treatments, and telehealth. That means more insurance eligibility checks and tighter claims management to prevent avoidable claim denials.
- Team workflows: Behavioral health providers coordinate across therapists, psychiatrists, case managers, and billing teams. Smooth practice management, managing records, and streamlined claims processing support patient care and operational efficiency.
- Payment behavior: Patient engagement and flexible payment options matter since recurring visits can lead to balances over time. You need tools that help collect payments and achieve timely reimbursements.
These differences affect revenue cycle management from start to finish. Knowing what you’re looking for helps you choose the best RCM software for your team, so they can focus on doing what they do best: caring for their patients.
Must-have features for RCM software in 2025
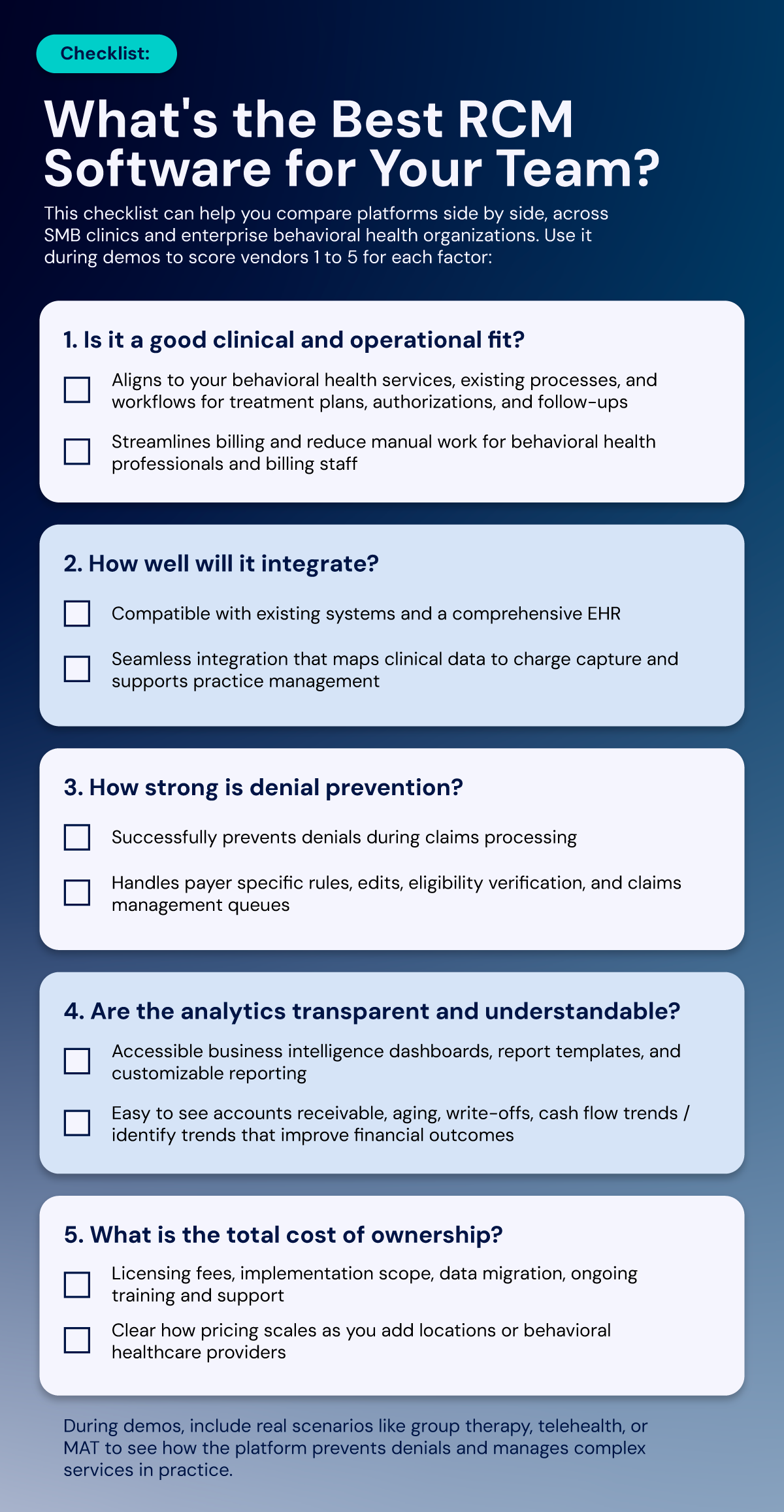
Here’s a closer look behind your checklist at key features you’ll need to keep your revenue cycle healthy and your team focused on patient care.
EHR and billing integration
A comprehensive EHR connection reduces duplicate work and supports seamless integration by linking treatment plans and clinical data directly to billing for accurate charge capture. Advanced tools can even scan provider notes to surface relevant diagnoses and suggested codes, which helps minimize errors.
If you want a single hub for EHR and RCM, explore EHR and billing integration options.
Eligibility and authorization automation
Real-time insurance verification prevents downstream denials, while automated checks against payer-specific rules during claims processing improve first-pass acceptance and speed up reimbursements.
Denial prevention and claims management
Built-in edits, denial management workflows, and clearinghouse tracking identify issues before they affect accounts receivable. Smart rules for modifiers, frequency limits, and place-of-service codes reduce rework and administrative burden.
Reporting, analytics, and BI
Customizable reporting and business intelligence tools provide detailed insights into financial performance and patient outcomes. Dashboards with predictive analytics make it easier to track denial rates, AR aging, write-offs, and payment posting speed, so you can identify trends and improve cash flow.
Patient financial experience
Clear statements, self-service portals, and flexible payment options support cash flow while improving the patient experience. These tools reduce staff workload and help patients stay engaged with their care.
Security, compliance, and controls
Strong platforms protect both clinical and financial data with role-based access, audit trails, consent management, and encryption. Look for vendors that also provide secure data migration, training, and ongoing support.
Fit for behavioral health services
The system should support the full range of behavioral health services, including individual therapy, group visits, MAT, and care coordination. Diagnostic support and decision-making aids further reduce errors and improve billing accuracy.
What’s the best RCM software for behavioral health?
The best platform is the one that fits your model, supports your revenue cycle end to end, and consistently drives timely reimbursements with low rework. For many teams, that means a comprehensive solution that connects clinical and billing workflows, automates eligibility checks, and provides clear analytics.
See How an Integrated RCM + EHR Improves Cash Flow
Get a live, 20-minute walkthrough tailored to your workflows.
RCM software FAQs
Should I use separate billing tools or an integrated platform?
Separate tools can work, but they often add handoffs, duplicate data entry, and more claim denials. An integrated platform with EHR and billing links reduces administrative tasks, ties treatment plans to charges, and helps you minimize errors. This usually improves operational efficiency, cash flow, and patient care. If you want to see how integration can help your organization, review EHR and billing integration options and our behavioral health RCM software overview.
How does RCM software handle compliance and HIPAA requirements?
RCM software should protect both clinical and financial data with built-in security controls. Look for platforms that use encryption, role-based access, and audit logs to safeguard patient information. HIPAA compliance means the system aligns with the HIPAA Security Rule, and it should also support consent management for services that require special authorizations. During implementation, confirm that vendors provide secure data migration and ongoing training so your team can adopt new features safely.
Suggested reading: Why HIPAA-Compliant RCM Matters for Therapy Centers
What reporting and analytics features should behavioral health leaders look for?
Behavioral health practices need more than basic financial reports. Strong RCM software should include business intelligence dashboards with filters for provider, location, payer, and service type, so leaders can quickly identify trends. Customizable reporting helps you track key metrics like denial rates, AR aging, write-offs, and payment posting speed. Quality reporting also links documentation and coding accuracy to patient outcomes and reimbursement, giving leaders insight into both financial performance and care quality.
How do I compare RCM platforms?
Your choice should help you streamline operations, reduce errors, and keep your team focused on care. Here’s a step-by-step to-do list:
- Map your revenue cycle, from patient intake and insurance eligibility to claims processing, payment posting, and accounts receivable follow-up.
- Build a demo script: Include your top services, complex billing codes, and authorizations. Ask vendors to show how they prevent claim denials and collect payments.
- Check analytics: Confirm you get business intelligence, customizable reporting, and predictive analytics to spot denial patterns.
- Validate security and compliance: Ask about data security, consent management, and audit logs.
- Model total cost: Include licensing fees, implementation, data migration, training, and support.
Explore our behavioral health RCM software by scheduling a demo.

